Many people do not know what blood type they have because it is not a test that is routinely performed. However, all mothers-to-be have it tested on a mandatory basis in order to respond appropriately in case of the possibility of a serological conflict. Parents often wonder what blood type the child will have. What is the inheritance of blood type? What consequences can a serological conflict have?
In Poland, according to statistics, the most common blood type is A Rh+, present in 1/3 of the population. The second place is occupied by the 0 Rh+ group, and the third by the B Rh+ group. The least common is AB Rh-, which only 1% of Poles have. Knowledge of blood types is essential when preparing for surgery, transfusions, but also in the prevention of serological conflict during pregnancy.
Child’s blood type vs. Parents
There are 4 basic blood types: 0, A, B and AB. These terms tell us what antigen is present on the surface of the blood cells in a person. In addition, the Rh factor, otherwise known as the D antigen, is always distinguished. If it is not present a person is “Rh negative.” Otherwise, she is “Rh positive.” Both of these systems, both ABO and Rh are very important among others. Before organ transplantation, but also during pregnancy. These are not the only systems, because thanks to the presence of numerous antigens, there are many more blood group systems in humans. These include. Kell, Lewis or Duffy system, but are not used most often in the daily practice of describing blood type.
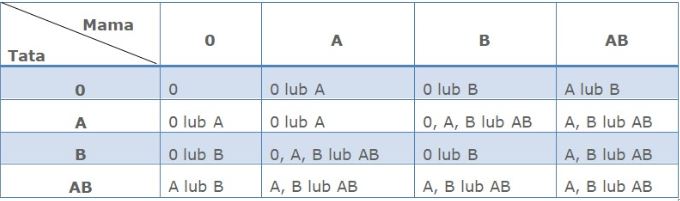
What ABO blood type a child will have is determined by the genes passed down from the Parents. There are three main gene variants, the so-called. alleles, different combinations of which will determine the blood type: these are the so-called. A, B, and 0 alleles. Each mom and dad-to-be, however, has only two of them, and passes on only one-at random-from the pair of alleles she has-to her offspring. If the child receives from the mother and from the father one allele each of 0-it will have blood type 0. If the child receives from one Parent the A or B allele, and from the other the 0 allele-he will have group A or B, respectively. If from, for example, the mother receives variant A, and from the father the B allele (two others)-the result of the child’s blood group will show group AB. When both the father and mother receive the same gene variant (two times A or two times B, respectively), the child will have blood type A or B.
Group A holders have the A antigen on the surface of their red blood cells, group B holders have the B antigen, group AB holders have both antigens, group 0 holders have no antigen. The antigens of the baby’s ABO groups are formed already in the womb – on average in 5.-6. week of fetal life, however, their full development occurs during 6- 18 months after birth. It is worth noting that at the same time in the plasma of each of us there are antibodies directed against red blood cell antigens, which we do not have on our own blood cells, for example, a person with blood type A does not have the surface of his erythrocytes antigen B, so anti-B antibodies can be found in his plasma.
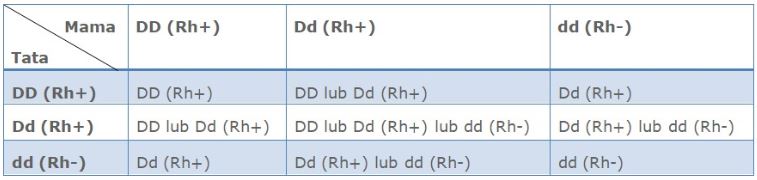
In the case of the Rh system, the presence of the D antigen is decisive. If both Parents have Rh- blood type, the child will definitely be Rh- as well, since the D antigen, which determines the Rh+ type, will not be passed on.
Baby’s blood type calculator
If you, as parents-to-be, know your blood type, check what blood type your child may have:
LAYOUT AB0
rh system
Blood type and serological conflict
Serological conflict most often occurs in the Rh system. It occurs when a woman has the blood type Rh-(meaning she does not have the D antigen on her blood cells) and the child Rh+(has the D antigen on his blood cells). However, there are possible conflicts in other arrangements. In the course of the conflict, maternal immune antibodies are formed against the baby’s antigens. This leads to hemolysis (breakdown of erythrocytes) and anemia in the fetus. They, in turn, can lead to hypoxia, organ damage, generalized edema and, in the absence of specialist intervention, intrauterine death of the baby.
To avoid this, every pregnant woman is ordered an indirect antiglobulin test called Coombs Reaction at her first pregnancy appointment. Through it, the presence of immune antibodies in the mother’s blood is determined. If detected, they should be identified and their titers assessed. When the mother-to-be is Rh-negative and does not have anti-D antibodies in the Coombs’ test at the beginning of pregnancy, she must have this test repeated each trimester to monitor for immunization (antibody formation).
Nowadays, serological conflict is much less common than it used to be. This is due to the tests performed during pregnancy and the use of intra-pregnancy and postpartum prophylaxis with immunoglobulins.
Baby’s blood type- testing during pregnancy
To test the baby’s blood type, for example, a non-invasive free fetal DNA test can be performed. An invasive test such as cordocentesis is used to determine the fetal blood type, as well as the hemoglobin concentration. However, the more commonly used and now recommended by specialists as the test of choice for diagnosing the onset of fetal hemolytic disease is the Doppler flow study. The specialist assesses the maximum systolic velocity (PSV) in the baby’s middle cerebral artery (MCA) and compares it to the average for a given gestational age. If severe anemia is detected in a child due to a serological conflict, intrauterine transfusions are performed using therapeutic cordocentesis.
See also: Belly at 30 weeks of pregnancy. Which month is it?
Rate this article: